Pancreas transplant is a life-altering procedure that offers hope for people suffering from severe pancreatic diseases, particularly type 1 diabetes. For patients who are unable to manage their blood sugar levels with insulin or experience complications such as kidney failure, a pancreas transplant can provide a new lease on life. However, like any major surgery, the Pancreas transplant procedure involves careful consideration, preparation, and understanding of its benefits, risks, and long-term management. In this comprehensive guide, we’ll explore the fundamentals of pancreas transplant, including what it is, how it’s done, who is a candidate, and the benefits and risks associated with the procedure.
What is a Pancreas Transplant?
A pancreas transplant is a medical procedure in which a patient’s diseased or non-functioning pancreas is replaced with a healthy pancreas from a deceased donor. The pancreas is an essential organ that produces insulin, which regulates blood sugar levels in the body. In individuals with diabetes, particularly type 1 diabetes, the pancreas does not produce insulin, leading to high blood sugar levels and a range of serious health complications.
A pancreas transplant can restore normal insulin production, allowing patients to maintain stable blood sugar levels without the need for insulin injections. Often, this procedure is performed in combination with a kidney transplant, especially for patients suffering from diabetes-related kidney failure. However, a pancreas transplant may also be done without a kidney transplant for patients with well-functioning kidneys.
Why Is a Pancreas Transplant Performed?
The primary goal of a pancreas transplant is to restore normal blood sugar control in individuals with diabetes, especially those with type 1 diabetes. While a pancreas transplant can be a potential cure for type 1 diabetes, it is not recommended for everyone. Typically, it is offered to people who meet the following criteria:
- Severe Type 1 Diabetes Complications: Pancreas transplant is often considered for people with type 1 diabetes who experience severe complications, such as diabetic kidney disease, frequent and unpredictable blood sugar swings, or hypoglycemia unawareness.
- Insulin Independence: Patients who are unable to achieve adequate blood sugar control through insulin therapy and are facing life-threatening complications may be eligible for a pancreas transplant.
- Combination with Kidney Failure: For patients suffering from kidney failure due to diabetes, a combined pancreas and kidney transplant may be recommended, as it can address both issues at once.
- Age and Overall Health: While pancreas transplant can be an option for people of various ages, overall health plays a significant role in eligibility. Individuals with other serious health conditions may not be suitable candidates for the procedure.
What are the Different Types of Pancreas Transplants?
There are three primary types of pancreas transplants, which are chosen based on the patient’s medical condition and specific needs:
- Pancreas Transplant Alone (PTA): This transplant is performed in patients with type 1 diabetes who do not have kidney disease. It involves replacing the diseased pancreas with a healthy one to restore insulin production and improve blood sugar control.
- Pancreas-Kidney Transplant (PKT): This is the most common type of pancreas transplant, performed for patients with both type 1 diabetes and end-stage kidney disease (diabetic nephropathy). The transplant involves the replacement of both the pancreas and the kidneys, typically from a deceased donor.
- Simultaneous Pancreas and Kidney Transplant (SPK): This type of transplant involves a combined pancreas and kidney transplant performed simultaneously. It is typically recommended for individuals who have both type 1 diabetes and kidney failure. By transplanting both organs at the same time, patients may experience better outcomes and recovery.
The Pancreas Transplant Procedure
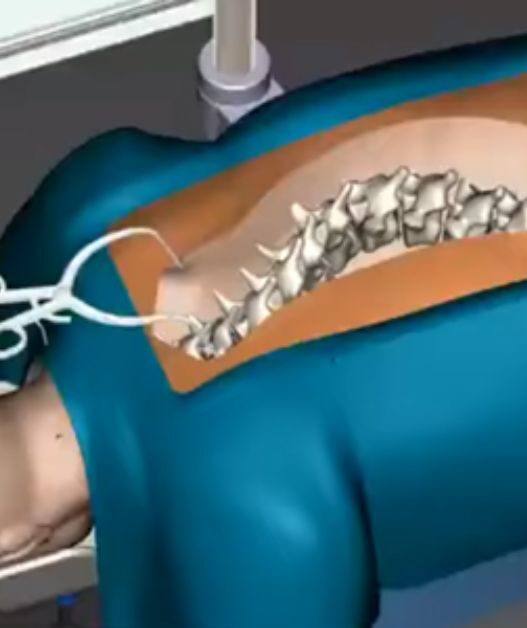
The pancreas transplant procedure is a complex and lengthy surgery, typically performed by a skilled transplant surgical team. Here is an overview of the process:
- Pre-Transplant Evaluation: Before a pancreas transplant, patients undergo a comprehensive evaluation to assess their overall health, kidney function (if applicable), and suitability for the procedure. This evaluation includes blood tests, imaging scans, and other diagnostic procedures.
- Organ Matching and Waitlist: Once a patient is deemed a candidate for a pancreas transplant, they are placed on a transplant waitlist. The donor pancreas must be compatible with the patient’s blood type, tissue type, and other factors. Since organ donors are limited, the waiting period can vary depending on availability.
- Surgical Procedure: During the transplant surgery, the diseased pancreas is removed and replaced with the donor pancreas. The donor pancreas is typically connected to the patient’s small intestine, where it can begin producing insulin to regulate blood sugar levels. In the case of a combined pancreas and kidney transplant, the kidney is also transplanted.
- Post-Operative Care: After the transplant, patients require intensive post-operative care, including monitoring for signs of infection, organ rejection, and other complications. Immunosuppressive medications are prescribed to prevent the body from rejecting the new pancreas, but these drugs also suppress the immune system, increasing the risk of infection.
- Long-Term Management: Following the transplant, patients need to follow a strict regimen of medications, including immunosuppressants, to prevent rejection. Regular follow-up appointments are required to monitor organ function and manage any potential side effects of the medications.
What are the Benefits of a Pancreas Transplant?
Pancreas transplant offers several potential benefits, particularly for patients with type 1 diabetes and severe complications. Here are some of the key benefits:
Improved Blood Sugar Control
The primary benefit of a pancreas transplant is the restoration of normal blood sugar control. After the transplant, the new pancreas begins producing insulin naturally in response to blood sugar levels, eliminating the need for insulin injections. This improves overall blood sugar control and reduces the risk of both high and low blood sugar levels.
Freedom from Insulin Injections
For individuals with type 1 diabetes, managing blood sugar levels often requires frequent insulin injections or the use of an insulin pump. After a successful pancreas transplant, patients can stop taking insulin entirely, which can greatly improve their quality of life and reduce the burden of daily diabetes management.
Improved Quality of Life
A pancreas transplant can significantly enhance a patient’s quality of life. With improved blood sugar control and the elimination of insulin dependency, patients often experience better overall health, more energy, and fewer diabetes-related complications. Many patients report a significant reduction in anxiety and stress associated with managing diabetes.
Reduction in Diabetes-Related Complications
Successful pancreas transplants can reduce or even reverse some of the complications caused by uncontrolled diabetes. This includes improvements in kidney function (especially for patients with diabetes-related kidney failure), a reduction in nerve damage (neuropathy), and a decrease in the risk of cardiovascular diseases, stroke, and eye complications.
Potential for Longer Life Expectancy
By improving blood sugar control and eliminating the risks of long-term diabetes complications, a pancreas transplant can potentially extend a patient’s life expectancy. For individuals with type 1 diabetes who experience severe complications, a pancreas transplant offers a chance for a healthier and longer life.
What are the Risks of a Pancreas Transplant?
While the benefits of a pancreas transplant are significant, it is important to be aware of the potential risks and complications:
Surgical Risks
As with any major surgery, a pancreas transplant carries risks such as infection, bleeding, and blood clots. Additionally, complications can arise during the procedure, particularly if the transplant is combined with a kidney transplant.
Organ Rejection
The body’s immune system may recognize the new pancreas as foreign and attempt to reject it. Rejection can occur immediately after the transplant (acute rejection) or over time (chronic rejection). To prevent this, patients must take immunosuppressive medications for life, which increase the risk of infections and other side effects.
Infections
Immunosuppressive medications reduce the body’s ability to fight infections, making transplant recipients more vulnerable to bacterial, viral, and fungal infections. Infections can complicate recovery and require additional treatment.
Graft Failure
Graft failure occurs when the transplanted pancreas stops functioning. This may happen due to rejection, infection, or other factors. If the pancreas fails, patients may need to resume insulin therapy and may require further medical treatment or another transplant.
Cancer Risk
Long-term use of immunosuppressive medications increases the risk of certain types of cancer, such as skin cancer and lymphoma. Patients need to be closely monitored for signs of cancer and take precautions to protect themselves from harmful UV radiation.
Conclusion
A pancreas transplant is a transformative procedure that offers significant benefits, particularly for individuals with type 1 diabetes who struggle with blood sugar control and diabetes-related complications. By restoring normal insulin production, a pancreas transplant can improve quality of life, eliminate insulin dependency, and reduce the risk of long-term health issues. However, it is important to understand the risks associated with the surgery, including the potential for rejection, infections, and the need for lifelong immunosuppressive medications.
If you are considering a pancreas transplant, it is essential to consult with an experienced transplant specialist to assess your eligibility and fully understand the benefits and risks involved. By taking the necessary steps and carefully weighing the options, patients can make informed decisions and potentially enjoy a healthier, insulin-free future.
Read This Article Also: