Electronic Health Records (EHR) have transformed how healthcare providers manage patient information. While EHR systems can streamline processes and improve patient care, integrating these systems into existing workflows can be challenging. Understanding the common hurdles of EHR integration is essential for healthcare providers looking to enhance their practices and deliver better patient outcomes. This blog will explore the key challenges healthcare providers face with EHR integration and provide actionable solutions to overcome them.
Understanding EHR Integration
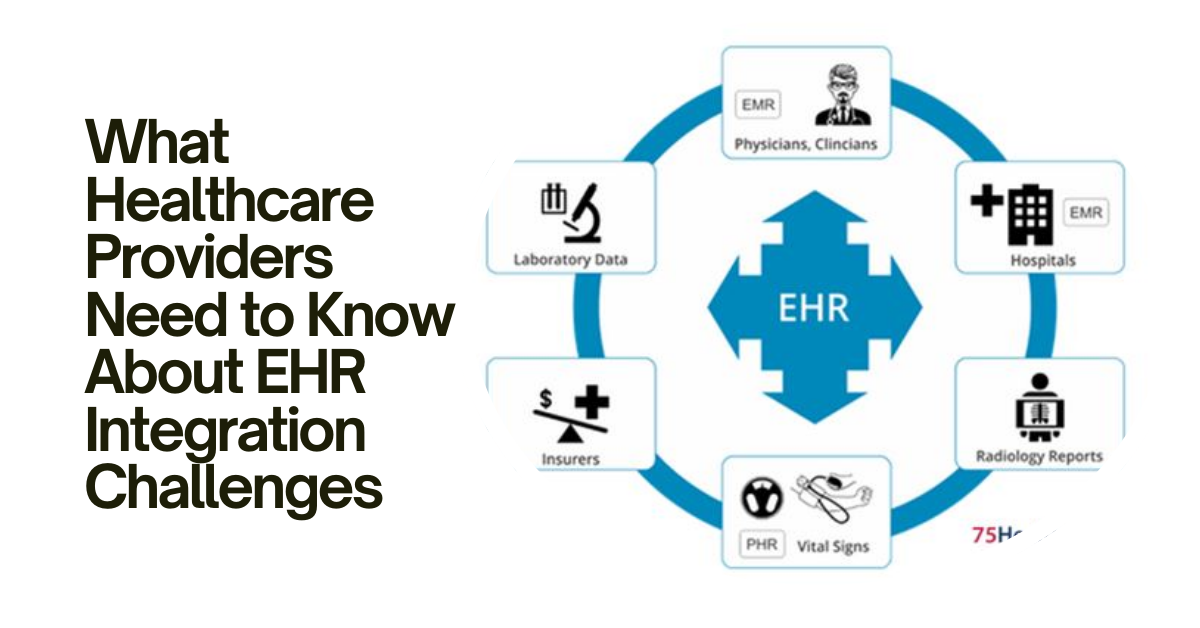
EHR integration refers to the process of connecting different health information systems and software applications to create a unified platform for managing patient data. This integration allows healthcare providers to access and share patient information quickly, which is crucial for delivering timely and effective care. However, the path to seamless EHR integration is not always straightforward. Various challenges can arise during the implementation and integration processes, impacting the overall efficiency and effectiveness of healthcare delivery.
The Importance of EHR Integration
EHR integration is crucial in modern healthcare for several reasons. First, it enhances communication between healthcare providers, ensuring that everyone involved in a patient’s care has access to the same information. This shared knowledge leads to better coordination of care, reducing the risk of errors and duplications. Second, integrated EHR systems can improve patient engagement by providing patients access to their health information, enabling them to participate actively in their care. Lastly, EHR integration helps streamline administrative processes, allowing healthcare providers to focus more on patient care rather than paperwork.
Note – Looking to enhance healthcare delivery? Explore EHR Integration Services for Healthcare Providers offered by BlueSecure. Streamline workflows, improve patient care, and achieve seamless data interoperability with a trusted partner. Contact BlueSecure today to discover how EHR integration can transform your healthcare practice.
Common Challenges of EHR Integration
1. Data Interoperability Issues
One of the most significant challenges healthcare providers face during EHR integration is data interoperability. Interoperability refers to the ability of different EHR systems to communicate and exchange data effectively. Unfortunately, many EHR systems use different data formats and standards, making it difficult to share information seamlessly. This lack of interoperability can lead to incomplete patient records, delayed treatment, and potential medical errors.
Healthcare providers must prioritize finding EHR solutions that support interoperability standards. Collaborating with vendors who focus on creating compatible systems can facilitate smoother integration. Additionally, ongoing training for staff on the importance of data interoperability can foster a culture of collaboration and communication among healthcare teams.

2. Resistance to Change
Resistance to change is a common issue in many organizations, and healthcare is no exception. Many healthcare providers are accustomed to traditional methods of record-keeping and may be hesitant to adopt new EHR systems. This resistance can stem from concerns about the learning curve associated with new technology, fears of decreased productivity during the transition, or a general discomfort with change.
To overcome this challenge, healthcare organizations should engage their staff early in the EHR integration process. Providing comprehensive training sessions and offering continuous support can help alleviate concerns and build confidence in using the new system. Additionally, showcasing the benefits of EHR integration, such as improved patient care and streamlined workflows, can motivate staff to embrace the change.
3. Data Migration Challenges
Data migration is a critical step in EHR integration, involving transferring patient data from old systems to new EHR platforms. However, this process can be fraught with challenges, including data loss, corruption, and discrepancies. Ensuring that all relevant patient information is accurately transferred is crucial for maintaining the continuity of care.
To mitigate data migration challenges, healthcare providers should invest in thorough planning and testing before the actual migration occurs. Conducting pilot tests can help identify potential issues and ensure that the migration process runs smoothly. Additionally, having a dedicated team to oversee the migration and address any problems that arise can significantly improve the overall outcome.
4. Compliance and Regulatory Concerns
The healthcare industry is heavily regulated, and compliance with various laws and regulations is paramount. EHR integration must adhere to these standards to protect patient privacy and ensure data security. Non-compliance can result in severe consequences, including legal penalties and damage to the organization’s reputation.
Healthcare providers must stay informed about current regulations related to EHR integration, such as the Health Insurance Portability and Accountability Act (HIPAA). Regular training on compliance for staff involved in EHR integration can help minimize the risk of violations. Furthermore, partnering with EHR vendors who prioritize compliance can ensure that the systems meet legal requirements.
5. Cost Implications
Implementing and integrating EHR systems can be a significant financial investment for healthcare providers. The costs associated with purchasing EHR software, training staff, and maintaining the system can add up quickly. Smaller practices, in particular, may struggle to allocate sufficient funds for a successful integration process.
To address cost implications, healthcare providers should conduct a thorough cost-benefit analysis before committing to an EHR system. Understanding the long-term benefits of improved efficiency and enhanced patient care can justify the initial investment. Additionally, exploring financing options or government grants can help offset some of the costs associated with EHR integration.
Best Practices for Successful EHR Integration
1. Conducting a Needs Assessment
Before embarking on the EHR integration journey, healthcare providers should conduct a needs assessment to identify their specific requirements and goals. Understanding what features and functionalities are essential for the practice can guide the selection of the right EHR system. Engaging with staff members to gather their input can also provide valuable insights into potential challenges and opportunities.
2. Involving Stakeholders
Successful EHR integration requires the involvement of all stakeholders, including healthcare providers, administrative staff, and IT professionals. Engaging these individuals early in the process fosters collaboration and ensures that everyone is on the same page. Regular meetings and updates can help address concerns and maintain transparency throughout the integration process.
3. Providing Comprehensive Training
Training is a crucial aspect of successful EHR integration. Healthcare providers should invest in comprehensive training programs that cover all aspects of the new system. This training should not only focus on technical skills but also emphasize the benefits of EHR integration for patient care. Ongoing training sessions can keep staff informed about updates and new features, ensuring that they feel confident in using the system.
4. Monitoring and Evaluation
After EHR integration, healthcare providers should monitor the system’s performance regularly. Collecting feedback from staff and patients can help identify areas for improvement and ensure that the system meets the organization’s needs. Evaluating the effectiveness of the EHR integration can also provide insights into potential future enhancements.
Conclusion
EHR integration is a powerful tool for healthcare providers, but it comes with its share of challenges. By understanding these challenges and implementing best practices, healthcare organizations can successfully navigate the integration process and ultimately improve patient care. The journey may be complex, but the benefits of a well-integrated EHR system far outweigh the difficulties. With careful planning, stakeholder involvement, and ongoing support, healthcare providers can leverage EHR integration to enhance their practices and deliver better outcomes for their patients.
For more insightful articles related to this topic, feel free to visit chemhubglobal.com